Ectopic Pregnancy is defined as a situation in which the fertilized egg implants outside the uterus. Cases of Ectopic pregnancy have been rare which sometimes leads to non-identification of the signs of ectopic pregnancy. Gynecologist records say that the baby most often doesn’t survive in the case of ectopic pregnancy, but it is not impossible.
What exactly is an Ectopic Pregnancy?
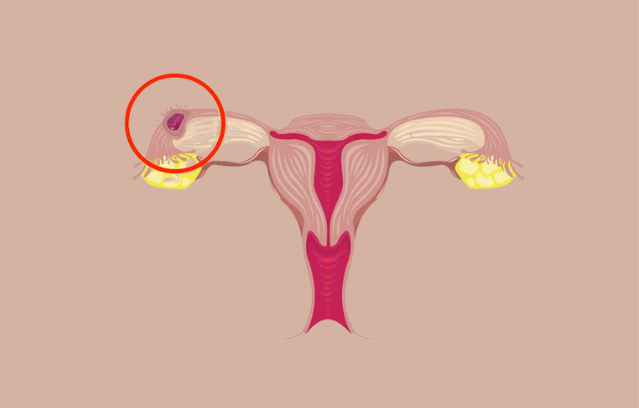
Extrauterine pregnancy is referred to as an ectopic pregnancy. When a fertilized egg implants in a structure that is incapable of supporting its growth, this occurs. Frequently, a pregnancy ectopic occurs in the fallopian tube (a pair of structures that connect the ovaries and uterus). An ectopic pregnancy can occasionally develop on an ovary or in the abdominal cavity.
This ailment poses a hazard to life. An ectopic pregnancy cannot be brought to term (until birth) and, if left untreated, could be deadly for the mother.
Where does Ectopic Pregnancy occur?
Anytime the fertilized egg implants outside of your uterus, the pregnancy is regarded as ectopic. The egg is intended to pass via your fallopian tubes and embed itself in the uterine wall, where it can start to develop. The egg implants in one of the structures along the route during an ectopic pregnancy. The fallopian tubes are the location where this can occur most frequently.
The majority of ectopic pregnancies, also known as tubal ectopic pregnancies, occur here. Additionally, a fertilized egg may implant on additional abdominal organs. Compared to ectopic pregnancies in fallopian tubes, this one is more uncommon.
How Serious is an Ectopic Pregnancy?
A medical emergency is an ectopic pregnancy. The uterus is specially designed to accommodate a developing fetus. As the fetus develops, it is an organ that can extend and enlarge. The fallopian tubes in your body are not as flexible. As the fertilized egg grows, it may burst.
You may endure significant internal bleeding when this occurs. This poses a hazard to life. To prevent damage to the fallopian tube, other organs in the abdominal cavity, internal bleeding, and death, an ectopic pregnancy needs to be treated straight away.
After an ectopic pregnancy, Will my pregnancy continue?
Unfortunately, a fetal death results from an ectopic pregnancy. It is unable to endure outside of the uterus. To save the mother’s life, an ectopic pregnancy must be treated right away. There may be significant internal bleeding if the fallopian tube ruptures after the egg have been implanted there. Maternal death may result from this.
Ectopic Pregnancy Causes
The majority of the time, factors that hinder or speed up the migration of the egg via the fallopian tube and into the uterus are what lead to an ectopic pregnancy. How can I tell if I might be having an ectopic pregnancy or how can you say the clear ectopic pregnancy causes?
Your chances of getting an ectopic pregnancy may arise due to several risk factors. A characteristic or action that raises your chances of contracting a disease or condition is called a risk factor. You might be more likely to experience an ectopic pregnancy if you’ve had:
- An ectopic pregnancy in the past.
- A history of pelvic inflammatory disease (PID), an infection that can lead to the formation of scar tissue in your cervix, uterus, and fallopian tubes.
- Surgery on your pelvic organs or on your fallopian tubes (including tubal ligation, often known as having your tubes tied).
- A background of infertility
- In vitro fertilization is used to treat infertility (IVF).
- Endometriosis.
- Sexually transmissible diseases (STIs).
- When a child is conceived, there is an intrauterine device (IUD) in place as a method of birth control.
- A background of smoking.
- As you age, your risk may also go up. Compared to younger women, women over 35 are more at risk.
- Many women who have an ectopic pregnancy do not have any of the risk factors mentioned above.
Signs of Ectopic Pregnancy
Early signs of an ectopic pregnancy can resemble usual pregnancy symptoms quite closely. However, you can also encounter the following signs and symptoms of ectopic pregnancy:
- Uterine bleeding
- Discomfort in your pelvis, lower back, and lower abdomen.
- Weakness or vertigo
- The pain and bleeding from a ruptured fallopian tube may be severe enough to produce additional symptoms.
These may consist of:
- Fainting.
- Reduced blood pressure (hypotension).
- Shoulders hurt.
- Rectal force.
You might experience severe lower abdomen pain if a tube ruptures. You should call your doctor or visit the emergency department right away because this is a medical emergency. You can also seek online consultation help for more advice or if you notice signs of Ectopic pregnancy.
How is an Ectopic pregnancy diagnosed?
Usually, an ectopic pregnancy is discovered during a visit to your doctor’s office. The signs of Ectopic pregnancy differ. To find the ectopic pregnancy, your gynecologist will first do several tests to confirm the pregnancy. These tests consist of:
- A Urine test entails:- Urinating on a test strip, which is often shaped like a stick, ectopic pregnancy symptoms can be easily judged from a urine test.
- A blood test: Your healthcare practitioner may do a blood test to determine your body’s level of the hormone human chorionic gonadotropin (hCG). When a woman is pregnant, this hormone is produced. This is also referred to as your serum beta-hCG level.
- An ultrasound examination employs sound waves to produce an image of the inside organs and tissues of your body. The use of ultrasound during pregnancy is common. This test will be used by your doctor to determine where the fertilized egg has been implanted.
- A treatment strategy will be developed when your doctor has confirmed your pregnancy and identified the location of the fertilized egg’s implant. Treatment for ectopic pregnancy is crucial because it is a medical emergency.
You must visit the emergency department right away if your fallopian tube bursts to receive rapid medical attention. There is no time to wait for an appointment in those circumstances.
How soon after conception is an ectopic pregnancy discovered?
Early on in pregnancy, ectopic pregnancies are frequently found. The majority of instances are discovered in the first trimester (the first three months). By the eighth week of pregnancy, it is typically identified. The fertility specialist has their own views on it and it may vary from person to person.
How do you handle an ectopic Pregnancy?
An ectopic pregnancy may be treated in several ways. In some circumstances, your doctor could advise using a drug called methotrexate to stop the pregnancy’s progress. Your pregnancy will cease as a result. Your healthcare practitioner will inject you with methotrexate. Although less intrusive than surgery, this method does necessitate follow-up visits with your doctor so that your hCG levels may be checked.
After an ectopic pregnancy, is it possible to conceive again?
The vast majority of women who experience ectopic pregnancies go on to have subsequent, successful pregnancies. After having an ectopic pregnancy, your chances of having more are increased. It’s crucial to discuss the reasons for your ectopic pregnancy with your healthcare practitioner, as well as any risk factors you may have for developing another one in the future.
How long should I wait after having an ectopic pregnancy before trying again?
After receiving treatment for an ectopic pregnancy, you should talk to your healthcare professional about upcoming pregnancies. It’s usually advisable to wait about three months after therapy, even though pregnancy may occur rapidly. This gives your fallopian tube time to recover and lowers the risk of professionals about upcoming pregnancies.
Talk openly with your healthcare professional or you can also take help from IVF clinic about your views about future pregnancies. You can create a plan and talk about how to reduce any risk factors you may have together.